Opportunities for improving patient care for aortic stenosis in primary care
About the survey
70 PCPs in Saudi Arabia participated in an electronic survey to assess their comprehension of aortic stenosis, encompassing knowledge regarding symptoms, prevalence among patients and the severity of the disease.48
Respondent characteristics:
- Experience ranged from 5 to 20+ years
- 89% based in Riyadh
- 71% based at a primary care center
- 22% based at Medical City
- 4% working in a specialized or tertiary care hospital or involved with home care
Heart auscultation
Guidelines and recommendations on managing and treating VHD are critical for ensuring care for people with severe aortic stenosis. Heart auscultation should be part of standard check-ups, and PCPs must have the skills to auscultate patients.
- All respondents acknowledge the importance of having local guidelines/recommendations for identifying patient profiles for heart auscultation and managing patients with a heart murmur .
- 76% of respondents agree that heart auscultation should be part of the standard check-up for patients over 65 years old (although only around 40% of respondents currently auscultate most of their elderly patients).
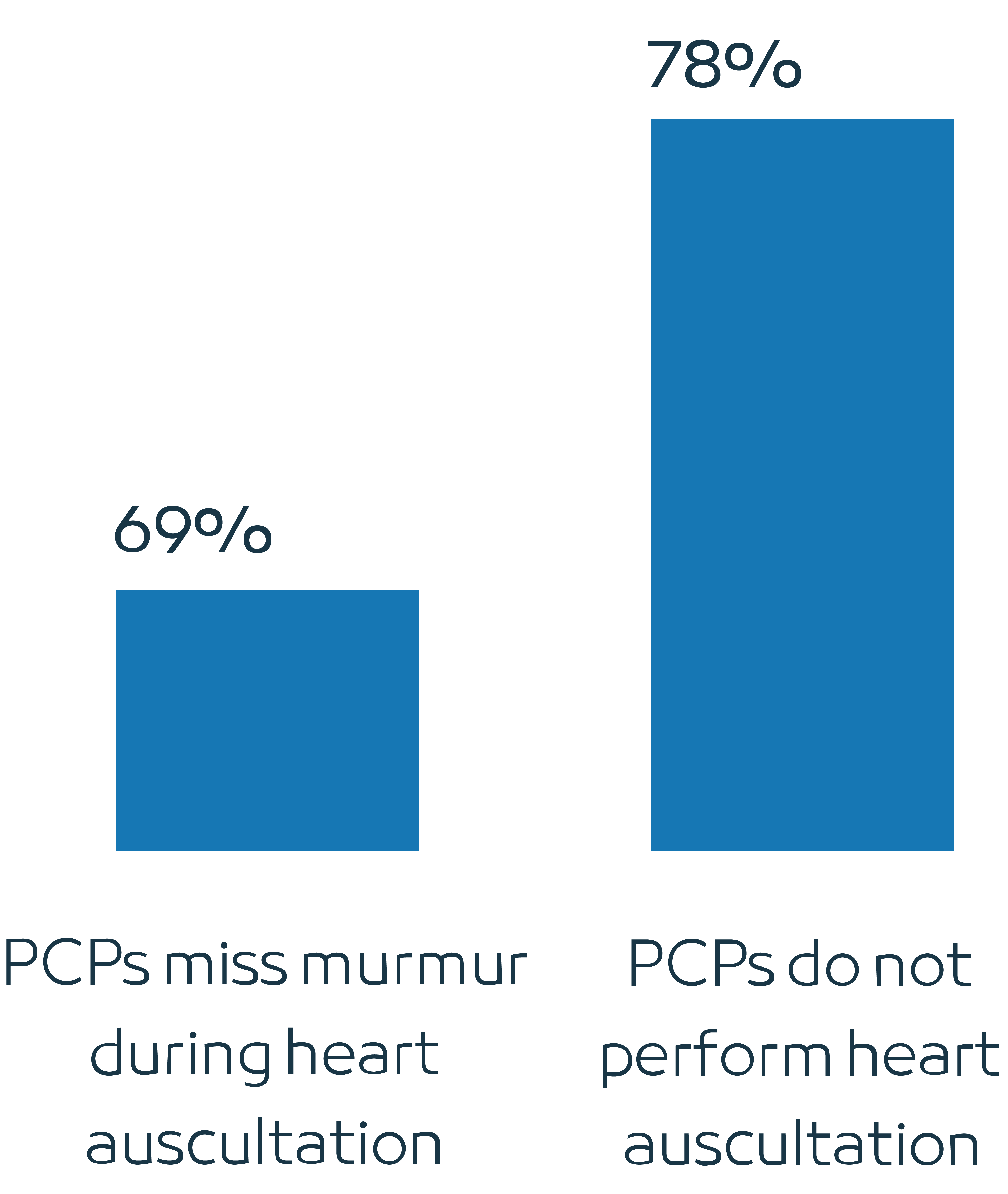
Heart auscultation is not a routinely performed test
- Only 40% of the respondents mentioned that they routinely auscultate patients over 65. In comparison, almost 90% of the respondents regularly measure blood pressure in their elderly patients.
Figure 4: Frequency of performing check-ups

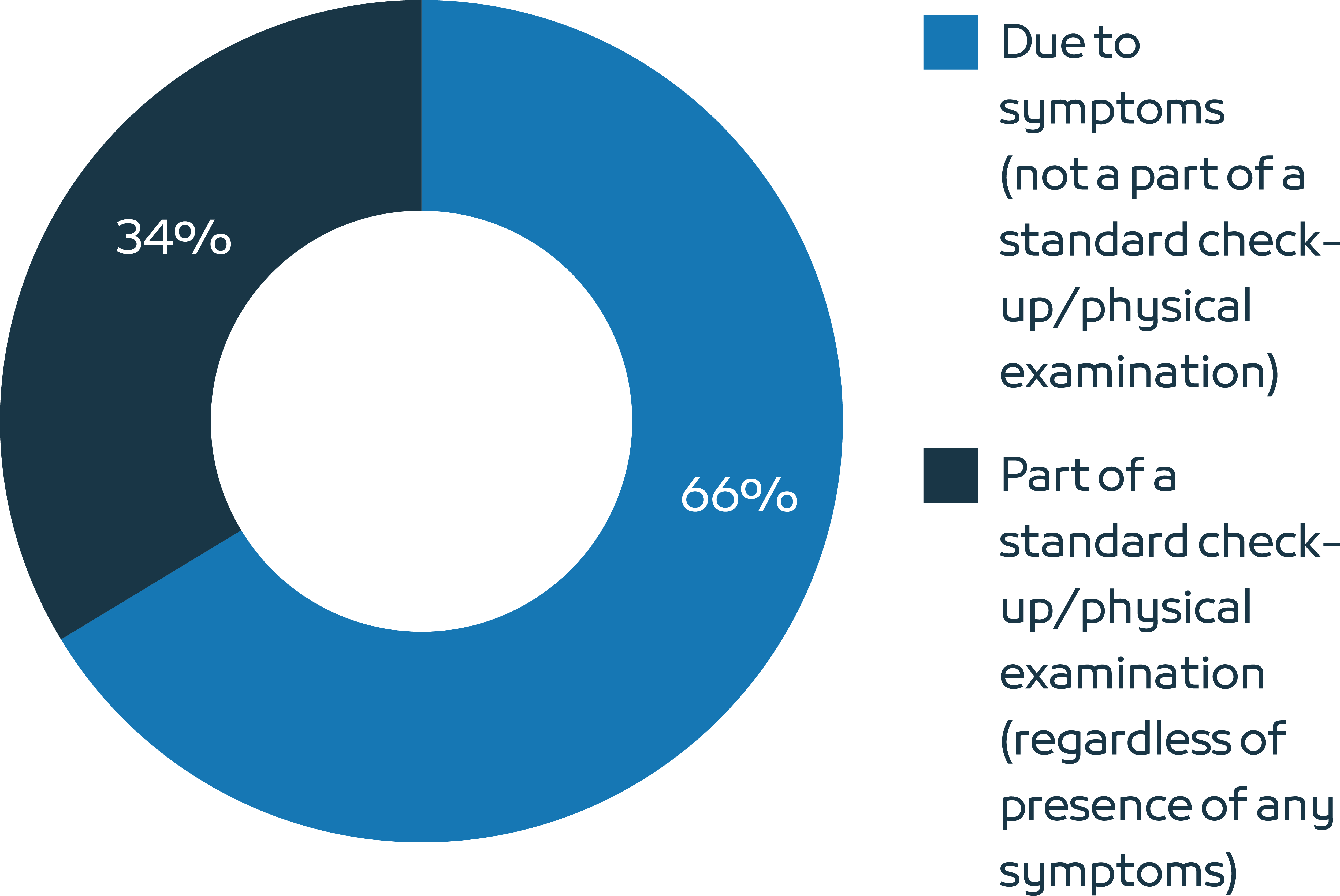
Symptoms are the main reason for performing heart auscultation On average,
- 66% of elderly patients are auscultated because of the presence of certain symptoms, namely palpitations, chest pain, or shortness of breath. This highlights the importance of ensuring that patients, their families, and PCPs are familiar with the symptoms of VHD.
- 34% of elderly patients are auscultated as part of a standard check-up/physical examination (regardless of the presence of any symptoms).
Figure 5: Heart auscultation
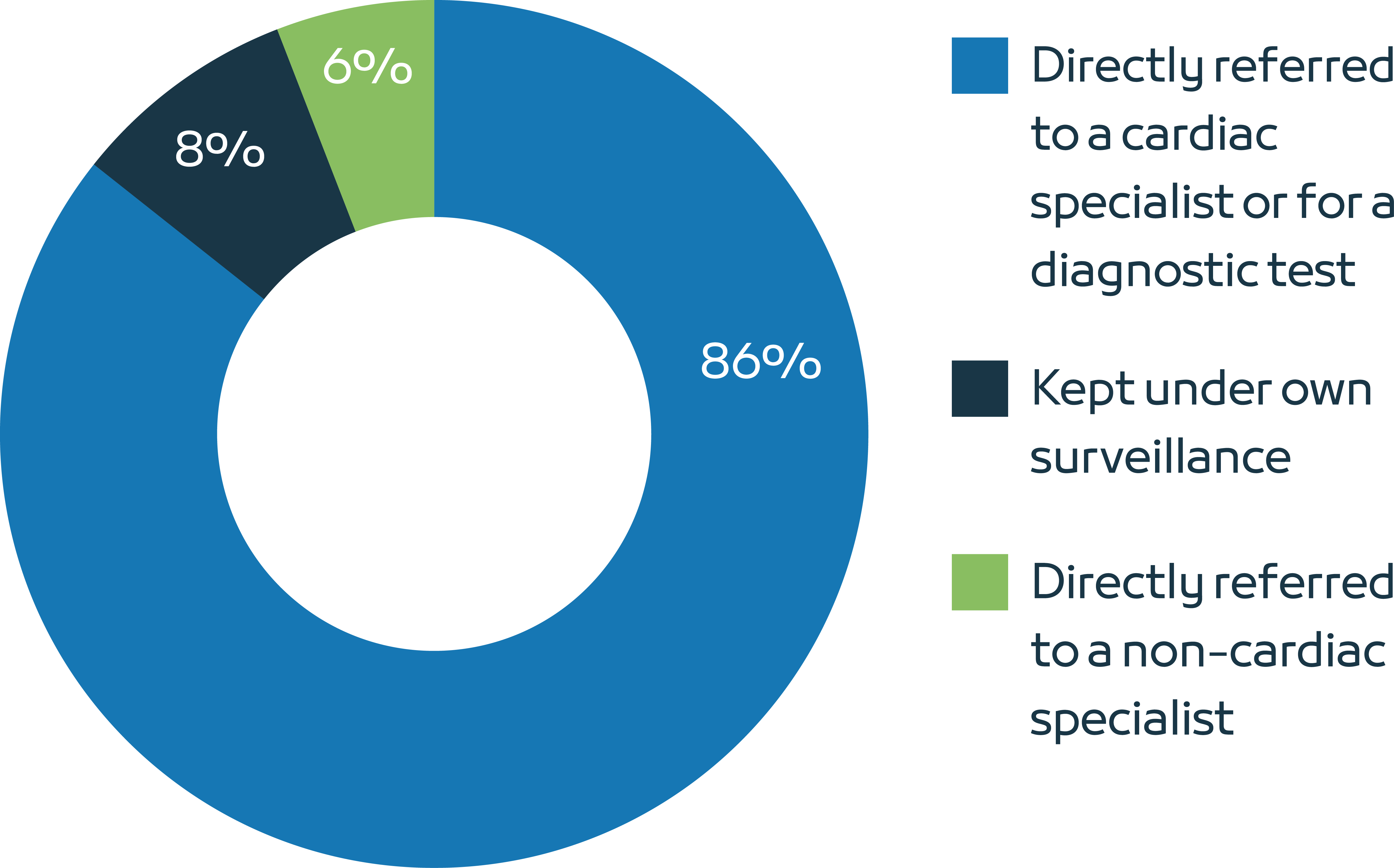
Referral after detecting a murmur
Clear referral pathways are essential for ensuring that elderly patients with detected heart murmurs receive timely and coordinated care from appropriate specialists, ultimately improving clinical outcomes and quality of life.
The majority of respondents report referring elderly patients for a diagnostic test (electrocardiogram or echocardiogram) or to a cardiac specialist for further investigation when a heart murmur is detected.
Around 14% of elderly patients with a heart murmur will not be referred to a cardiologist or for a diagnostic test.
Reasons for not referring a patient include: unclear referral network, patient’s personal preference, and long waiting time for referral.
Around 6% of patients with a heart murmur are referred to a non-cardiac specialist. Typically, these are patients who suffer from other comorbidities or patients who are already followed up by a cardiologist due to a previously detected heart murmur.
Figure 6: Referral of patients with detected heart murmur
Severe aortic stenosis
Annual check-ups play a crucial role in the management of patients with asymptomatic aortic stenosis by facilitating monitoring of disease progression, early detection of symptoms, risk assessment, and coordination of care.
Respondents suggest that asymptomatic patients with severe aortic stenosis should have a yearly check-up with a cardiologist, ideally every six months, and should undergo an electrocardiogram or echocardiogram annually.
- 80% of respondents agree that there is a low awareness of aortic stenosis among patients and caregivers about the disease and its symptoms and that there is underdiagnosis and undertreatment of patients over 65 years suffering from severe aortic stenosis.
- One in three respondents were unsure about how to categorize or assess the seriousness of a patient’s aortic stenosis.
- One in four respondents believe they do not have enough knowledge about the available interventions (SAVR, TAVI) for treating severe aortic stenosis.
Figure 7: The main reasons for underdiagnosis of severe aortic stenosis are connected with PCPs